Genomic medicine has the potential to revolutionize patient care. Yet, major questions remain about the value it provides and its impact overall health care expenditures. Advocates hope that genomic medicine will help control expenditures by streamlining diagnostic processes, informing selection and dosing of treatments, and identifying at‐risk individuals to facilitate targeted prevention. The price of genomic medicine, however, remains high relative to most other tests; and some tests, such as genomic sequencing may identify secondary findings that initiate a cascade of confirmatory and follow‐up testing that may not be warranted. These uncertainties pose major barriers to the practice of genomic medicine, making many payers reluctant to cover services.
 Our Econogenomics Working Group brings together a diverse set of researchers with a variety of clinical and scientific expertise. Our economic modeling core, led by Dr. Ann Wu, uses a variety of modeling approaches to project the medical and financial consequences of genomic medicine, including the use of pharmacogenomic testing to inform medication choices and the use of sequencing as an adjunct to standard newborn screening. Our clinical core, led by Dr. Kurt Christensen, conducts economic analyses alongside prospective clinical studies to better understand the full costs of sequencing and to collect real-world data about health care utilization and clinical outcomes following genomic tests. Together, our mission is to understand the economic impact of translating genomic advances into clinical practice.
Our Econogenomics Working Group brings together a diverse set of researchers with a variety of clinical and scientific expertise. Our economic modeling core, led by Dr. Ann Wu, uses a variety of modeling approaches to project the medical and financial consequences of genomic medicine, including the use of pharmacogenomic testing to inform medication choices and the use of sequencing as an adjunct to standard newborn screening. Our clinical core, led by Dr. Kurt Christensen, conducts economic analyses alongside prospective clinical studies to better understand the full costs of sequencing and to collect real-world data about health care utilization and clinical outcomes following genomic tests. Together, our mission is to understand the economic impact of translating genomic advances into clinical practice.
Working Group Members
Carrie Blout Zawatsky, MS, CGC
Kurt Christensen, PhD
Kenneth Freedberg, MD
Robert C. Green, MD, MPH
Christine Lu, PhD
Natasha Stout, PhD
Mark Williams, MD
Ann Wu, MD
Jennifer Yeh, PhD
Areas of Focus
Pharmacogenomics: Pharmacogenomics is the study of how a person’s genetic makeup affects how medications and medication doses are likely to work best for a particular person or which individuals are more likely to suffer adverse consequences. Pharmacogenomic tests have the potential to improve resource allocation by improving targeting of treatments so that individuals at risk of having adverse responses to medications or not responding to medications can avoid them, thereby reducing healthcare costs. With thousands of pharmacogenomic tests under development and many becoming available for clinical use, it is becoming increasingly important to understand the costs and benefits of these tests so that their potential for widespread use can be critically evaluated in ways that optimize their usefulness.
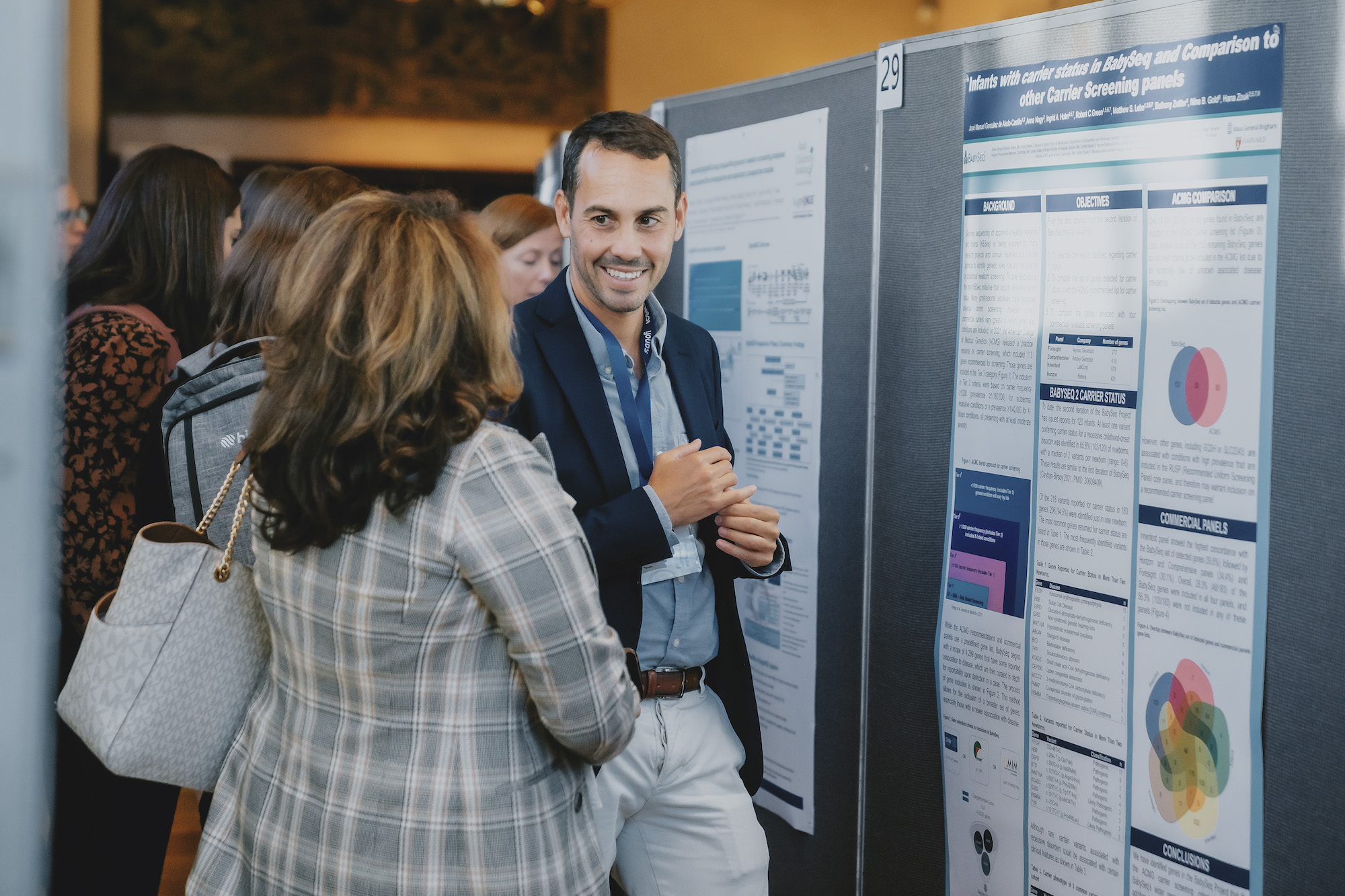
 Genome and Exome Sequencing: Genome and exome sequencing has increasing utility for diagnosing disease and informing treatment decisions. With costs decreasing rapidly, many thought leaders believe that such sequencing will become commonplace, even among healthy individuals. Yet, the benefits and harms of integrating sequencing into the care of many populations are still unclear, as are the cost implications. Capitalizing on our experiences with high-profile clinical trials such as the MedSeq Project and BabySeq Project and our strong relationship with the Laboratory for Molecular Medicine, our group is using a combination of modeling and clinical studies to examine the costs and consequences of integrating genome and exome sequencing into a variety of clinical settings.
Genome and Exome Sequencing: Genome and exome sequencing has increasing utility for diagnosing disease and informing treatment decisions. With costs decreasing rapidly, many thought leaders believe that such sequencing will become commonplace, even among healthy individuals. Yet, the benefits and harms of integrating sequencing into the care of many populations are still unclear, as are the cost implications. Capitalizing on our experiences with high-profile clinical trials such as the MedSeq Project and BabySeq Project and our strong relationship with the Laboratory for Molecular Medicine, our group is using a combination of modeling and clinical studies to examine the costs and consequences of integrating genome and exome sequencing into a variety of clinical settings.
Reimbursement: Given the uncertainties about the health and financial impact of many genomic tests, payers are often reluctant to cover genomic services. Our group has ongoing efforts to engage with payers to educate them about how genomic tests work and their potential consequences for patients, physicians, and health care systems. As part of this dynamic, we also aim to better understanding the payer perspective to direct future research in ways that can reduce uncertainties and improve their decision making about reimbursement.
For more detailed information about the Econogenomics Working Group, visit the links below or email us at g2p@bwh.harvard.edu.